Hossein Aghaei, Behrouz Torabi, Parya Abdolalizadeh, Homa Vaghfipanah
Purpose: Daily cleansing of eyelids is very important to carry out a successful blepharitis treatment.
However, there are no therapeutic guidelines for blepharitis. The aim was to compare the symptomatic
relief of anterior blepharitis using Blephamed eye gel, a cosmetic product, versus standard treatment.
Methods: The study was a prospective, interventional open label clinical trial at a university‑based hospital.
The test population was subjects aged 18–65 years who presented with mild to moderate anterior blepharitis.
Eyelid hygiene was applied twice a day. At each visit, a detailed assessment of symptomatology was carried
out. A two‑way repeated measure mixed model ANOVA was used to compare two groups by time. Results:
In total, 61 patients with mean age of 60.08 ± 16.69 years were enrolled in the study including 30 patients in
standard group and 31 patients in Blephamed group. Two groups did not differ in terms of age (P = 0.31) and
eye laterality (P = 0.50). The baseline scores of erythema, edema, debris, and symptoms as well as total score
were similar between two groups (all P values >0.50). Two groups became different for all these parameters at
day 45 (all P values <0.001). Significant interaction was detected between time and intervention groups for all
severity parameters of blepharitis as well as total score (all P values <0.001). Conclusion: Eyelid hygiene with
Blephamed more significantly decreased symptoms of anterior blepharitis compared to standard treatment.
Key words: Blephamed, Blepharitis, cleansing gel, eyelid hygiene, tea tree oil
Blepharitis is a frequently encountered chronic inflammatory
disorder of the eyelid margin.[1] Blepharitis is divided into
anterior and posterior blepharitis.[1] In anterior blepharitis,
anterior lid margins and the region of the eyelashes are involved,
while posterior blepharitis happens due to meibomian glands
dysfunctions.[1] The etiology of anterior blepharitis is not
completely determined yet, but three convergent pathways
have been proposed: 1) direct bacterial infection, 2) exotoxin
hypersensitivity, and 3) delayed cell‑mediated immune
hypersensitivity response.[1] These processes lead to ocular
surface inflammation, itching, redness, burning, dryness, and
blurred vision.[2,3] In clinical exam of patients with anterior
blepharitis, scaly lashes, collarets around eyelashes as well
as eyelash loss, misdirection and depigmentation may be
observed. Blepharitis can also result in complications such
as marginal ulceration of cornea, conjunctival or corneal
phlyctenulosis.[1]
Daily cleansing of eyelids is very important to carry out
a successful blepharitis treatment. However, there are no
therapeutic guidelines for blepharitis.[3] Various eyelid cleansing
products are becoming commercially available to aid in removal
of lash debris. Majority of them contain tea tree oil(TTO) which
is a natural oil extracted from the leaf of Melaleuca alternifolia.
TTO has antibacterial, antifungal, antiviral, and antiprotozoal
properties in addition to anti‑inflammatory effects.
————————————————————————————————————-
Eye Research Center, The Five Senses Institute, Rassoul Akram
Hospital, Iran University of Medical Sciences, Tehran, Iran
Correspondence to: Dr. Parya Abdolalizadeh, Eye Research Center,
Rassoul Akram Hospital, Sattarkhan Niayesh St., Tehran, Iran.
E‑mail: Payaabdolalizadeh@gmail.com
Received: 03‑Oct‑2022 Revision: 10‑Feb‑2023
Accepted: 12‑Feb‑2023 Published: 17May2023
[4] The TTO‑impregnated wipes with 2%–4% concentration,[5‑7] the
TTO foam formulation with 2%,[8] and the TTO eyelid gel
with 4%[9] cause an improvement in overall ocular discomfort,
in addition to a decrease in the characteristic ocular signs of
blepharitis. The Scientific Committee on Consumer Products
in European Union considered that at concentrations above
5%, TTO is more likely to induce skin and eye irritation.[10]
Therefore, Blephamed is an advanced cleansing gel formulation
including 2% TTO which was developed to avoid the irritation
and to sensitize the potential of high amounts of TTO. Current
study was carried out in order to test the hypothesis that
Blephamed can control blepharitis symptoms, damage, and
inflammation while providing effective cleansing of eyelashes.
The aim of the study was to investigate the efficacy and safety
of the advanced gel and to compare its effectiveness with the
standard treatment.
Methods
This is a prospective, randomized, controlled parallel‑group,
open‑label clinical study on patients with anterior blepharitis
presented to the cornea clinic of the senior author at a
university‑based hospital from March 2021 to August
———————————————————————————————————————–
This is an open access journal, and articles are distributed under the terms of
the Creative Commons Attribution‑NonCommercial‑ShareAlike 4.0 License,
which allows others to remix, tweak, and build upon the work non‑commercially,
as long as appropriate credit is given and the new creations are licensed under
the identical terms
For reprints contact: WKHLRPMedknow_reprints@wolterskluwer.com
Cite this article as: Aghaei H, Torabi B, Abdolalizadeh P, Vaghfipanah H.
Comparison of the effect of tea tree oil eye gel with standard treatment
in patients with anterior blepharitis: An open‑label clinical trial. Indian J
Ophthalmol 2023;71:218892.
2021. The study was registered as a clinical trial at Iranian
Registry of Clinical Trial (https://www.irct.ir) (Registration
number: IRCT20181102041528N1) and Center for Research
and Training in Skin Disease and Leprosy (https://crtsdl.tums.
ac.ir) (Registration number:ج/4/23/341 (as well as approved by
its Ethics Committee (IR.IUMS.FMD.REC.1400.117). The study
also adhered to the tenets of the Declaration of Helsinki and
conformed to the CONSORT checklist. After explaining the
purpose of the study and possible results, all patients provided
signed informed consent to participate in this study.
Study population
All patients with complaints of burning, stinging, and
heaviness sensations in the eyes were examined by an anterior
segment specialist. Patients with hyperemia, edema, and
telangiectasia of the anterior lid margin as well as scaling,
collarets, cylindrical dandruff, and oily secretion in the
eyelashes who aged between 18 and 65 years were enrolled in
the study. Patients with concomitant corneal ulcer, acute ocular
infection (bacterial, viral, or fungal), any clinically significant
lash or lid abnormality other than blepharitis, previous eyelid
surgery within 12 months before study, eyelid cellulitis, eyelid
hordeolum, moderate‑to‑severe dry eye, ocular surgery within
the last 3 months were not included. Moreover, subjects who
use systemic anti‑inflammatory drugs, are pregnant, are
nursing, are using contact lenses, and received topical treatment
other than artificial tear preparations within the last 2 weeks
were excluded from the study.
Study protocol
The patients were randomly assigned in 1:1 ratio to one of two
groups (standard‑treatment group and Blephamed group)
by an independent clinical research coordinator according
to a computer‑generated randomization list. Randomization
sequence was stratified with a 1:1 allocation. Duration of
treatment was two weeks. In Blephamed group, participants
were instructed to apply the gel to the eyelid and roots of the
eyelashes for 3–5 min, twice a day. Blephamed eye gel (Saya
Teb Mana Co., Tehran, Iran) contains TTO 2%, hyaluronic acid
0.2%, deionized water, glycerin, sodium pyrrolidone carboxylic
acid, vitamin B5, aloe vera extract, and ORONAL LCG (a mild
anionic surfactant). The eye gel was given for the patients free of
charge. Patients of standard‑treatment group were prescribed
topical erythromycin ointment (Sina Daru Co., Tehran, Iran)
per night and fluorometholone 0.01% (Sina Daru Co., Tehran,
Iran) eye drops three times a day. They are also instructed to
apply the heated compress to the eyelid for 3–5 min with a
slight pressure and then cleansing the eyelid margins with
baby shampoo, twice daily.
Clinical measurement
To evaluate degree of anterior blepharitis, both upper and
lower eyelids were observed with slit‑lamp biomicroscopy and
clinical measurements were conducted at baseline and days
14 and 45 of the treatment period. Clinical signs, including
erythema, edema, debris, and symptoms were evaluated
by an anterior segment specialist (HA). All of these items
scored on a 0–3 scale.[11] Erythema is graded as 0 for redness
at eyelash bases without eczema, 1 for pink appearance, 2 for
light red appearance or presence of eczema and, 3 for dark
red appearance.[11] Eyelash debris is scored 0 if no debris, 1 if
scattered, 2 if half, and 3 if most of the eyelashes have debris.[11]
Lid edema more than 1 mm is considered score 3, 0.5 to 1 mm
score 2, just noticeable score 1, and none score 0.[11] If patient is
asymptomatic, the symptom score is 0. Occasional, frequent,
and persistent symptoms are considered score 1, 2, and 3,
respectively.[11] Total score was calculated by summing up
scores assigned to each item. Participants were asked to contact
the clinic in case of any side effects.
Statistical analyses
SPSS software version 22 (SPSS, Inc., Chicago, IL, USA) was
used to perform analysis. A P < 0.05 was considered statistically
significant. Baseline characteristics of the two groups were
compared using a Chi‑square test (categorical variables) and
independent t‑test (continuous variables). A two‑way repeated
measure mixed model ANOVA was used to simultaneously
test the null hypotheses of the study: There is no interaction
between time and intervention (the two groups do not differ in
their degree of change in the blepharitis over time). Therefore,
we evaluated whether the two intervention affect the blepharitis
differently over time by considering intervention × time
interactions as our primary outcome measure. The changes of
blepharitis at the baseline and follow‑up examinations in each
group of the study (intragroup) were analyzed by one‑way
repeated measure ANOVA and post hoc tests. The sample size
was calculated based on the one‑way ANOVA formula using
G*Power software. By assuming ɑ =0.05, power = 80%, the
standardized Cohen effect size (f = 0.40), and a 10% dropout rate,
the final sample size of each group was estimated at 30 patients.
Results
In total, 61 patients with mean age of 60.08 ± 16.69 years were
enrolled in the study including 30 patients in standard group
and 31 patients in Blephamed group. More than 60% (63.9%,
39/61) were females. The two groups did not differ in terms of
age (P = 0.31) and eye laterality (P = 0.50) [Table 1]. However,
the percentage of females was higher in the standard
group (P = 0.003).
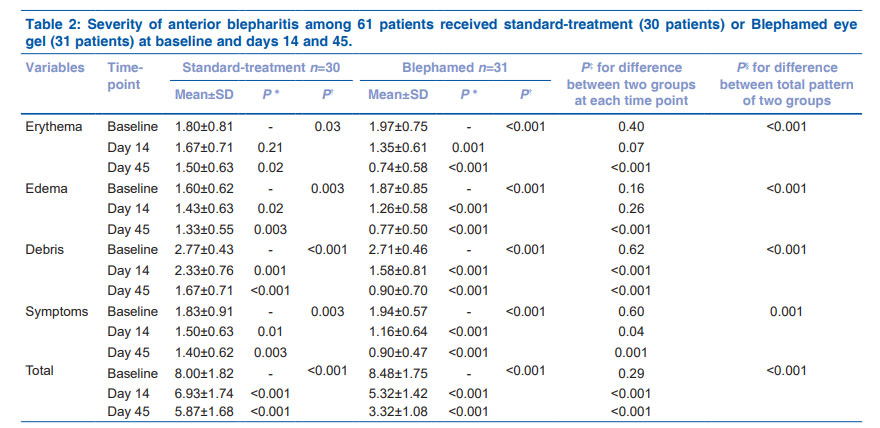
The baseline scores of erythema (P = 0.40), edema (P = 0.16),
debris (P = 0.62), and symptoms (P = 0.60) as well as total
score (P = 0.29) were similar between two groups [Table 2].
At day 14, eyelid erythema (P = 0.07) and edema (P = 0.26)
of two groups were also similar while Blephamed group
had less debris (P < 0.001), symptoms (P = 0.04) and total
score (P < 0.001) [Table 2]. Two groups became different for all
these parameters at day 45 [Table 2]. In two groups, all severity
parameters of blepharitis as well as total score decreased
significantly by time [Table 2].
Based on the mixed model analysis, significant interaction
was detected between time and intervention groups for all
severity parameters of blepharitis as well as total score (all
P values < 0.001); therefore, the two treatment groups differed
—————————————————————————————————
Table 1: Baseline characteristics of 61 patients with anterior
blepharitis received standard‑treatment (30 patients) or
Blephamed eye gel (31 patients)
Variables Standard‑treatment Blephamed P
Age (years) 57.78±17.76 62.23±15.57 0.31*
Sex (Female %) 83.3% (25/30) 45.2% (14/31) 0.003†
Laterality (OD%) 63.3% (19/30) 54.8% (17/31) 0.50†
in terms of changes in severity parameters of blepharitis over
time [Table 2]. Figs. 1 and 2 showed that Blephamed group
had more reduction of disease severity than standard group.
No adverse event has been observed in Blephamed group.
Discussion
Current study tried to compare the effect of Blephamed with
standard treatment in patients with anterior blepharitis.
Although the severity of blepharitis has been reduced in two
groups, the improvement was more pronounced in Blephamed.
Blepharitis is a multifactorial disease. The bacteria overload
and the inflammation due to a load of bacteria, especially
staphylococcal or seborrheic contamination, have a significant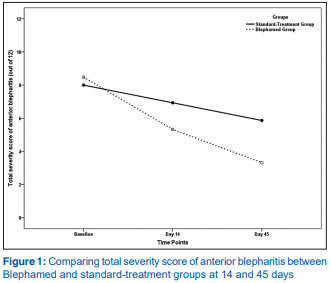
role in developing the disease.[1‑3] Chronic forms of anterior
blepharitis tend to reveal increased numbers of nonpathologic
flora.[1] Increased cell‑mediated immunity to S. aureus was
reported in nearly 40% of anterior blepharitis patients,
necessitating topical corticosteroid therapy.[12] In addition to the
bacterial etiology, the potential association between Demodex
infestation and blepharitis has also been recognized.[13] Lashes
with cylindrical dandruff are a pathognomonic sign of ocular
Demodex. Demodex has been found to localize in 50% of
patients even after cleaning the roots of the eyelashes with
baby shampoo for 1 year.[14]
Daily cleansing of eyelids is very important to carry out a
successful blepharitis treatment. Routine application of eyelid
hygiene removes debris, softens thickened secretions, removes
ciliary dandruff and cleans the eyelid margin.[2,3] However, there
*One‑way ANOVA repeated measure post hoc tests for comparing with baseline; †: One‑way ANOVA repeated measure Greenhouse–Geisser correction,‡
Independent student t‑test, § One‑way ANOVA repeated measure Greenhouse–Geisser correction to evaluate the interaction between time and intervention
are no therapeutic guidelines for blepharitis.[3] In the standard
treatment, patients are instructed to perform hyperthermic lid
compress, clean the eyelids with wet, warm gauze applied to
closed eyelids for several minutes to remove pathogens and
secretion along the eyelid margin.[15] Topical and systemic
antibiotics, topical corticosteroids, and tear‑replacement therapy
are common adjunctive therapies for standard treatment.[15]
Various eyelid cleansing products are becoming
commercially available to aid in removal of lash debris
although, baby shampoo continues to be frequently used.[16‑18]
The comparative studies of soap, shampoo versus eyelid
cleansing products have revealed that both cleansing regimens
improve some symptoms.[19] It is in agreement with current
study. Nevertheless, eyelid cleansing products are preferred
by patients against baby shampoo and soap.[17,19,20] It could
be explained by increased ocular inflammation with baby
shampoo.[21] Furthermore, the preparation and storage of
the diluted baby shampoo solution is unlikely to be done by
patients accurately and in sterile conditions at home.[19]
The TTO is one of the main components of the eyelid
cleansing products. The most active component of TTO is
terpinen‑4‑ol, accounting for 40% of its composition, which
is the primary agent responsible for the Demodex killing
effect.[5] In in‑vitro studies, it has been shown that Demodex
is resistant to many antiseptic solutions, but is sensitive to
TTO.[22] TTO‑containing eyelid scrub has shown to be a useful
tool for encouraging patients to persist with eyelid hygiene
regimens.[23] TTO inhibits iNOS expression, NO production
and NF‑κB activation in human macrophages.[24] It also reduces
proinflammatory mediators including IL‑1β, IL‑1β, IL‑8, L‑17,
and TNFα levels in blepharitis patients.[25,26]
Various forms of TTO have been made to treat patients
with blepharitis. The TTO‑impregnated wipes with 2%–4%
concentration have comparable effect to 50% TTO.[5‑7] The TTO
cleansing wipes administered daily, cause an improvement
in overall ocular discomfort, in addition to a decrease in the
characteristic ocular signs of Demodex infestation.[6] Patients
found wipe form easy to use and convenient despite they felt
stinging upon application.[27] De Luca et al.
[28] showed that wet
wipes imbibed with a solution of TTO and hyaluronic acid as
well as aloe, natural anti‑inflammatories and antiseptics were
effective than standard treatment in patients with posterior
blepharitis. The composition of this product is similar to
Blephamed eye gel. A foam formulation with 2% TTO also
confirmed its ability to exert a broad‑spectrum antimicrobial
effect without causing ocular or skin irritation.[8] Eyelid gel
with 4% improves ocular symptoms of blepharitis in 90% of
Demodex positive patients after one‑month treatment.[9] In line
with previous studies, current study showed that Blephamed
eye gel with TTO concentration of 2% was also effective in
treatment of patients with anterior blepharitis.
Some side effects of high ratio of TTO as a bioactive
component in the eyelid cleansing formulations include contact
dermatitis, allergic reactions, and ocular irritation.[29] Some
organic compounds of TTO such as terpinolene, α‑terpinene,
ascaridol, and 1,2,4‑trihydroxymethane induce these
reactions.[5] The Scientific Committee on Consumer Products
in European Union considered that at concentrations above
5%, TTO is more likely to induce skin and eye irritation.[10] It
necessitates prudent clinical judgment surrounding therapeutic
benefits of TTO‑containing formulations and highlights the
need for elimination of the unwanted chemical ingredients
and concentration adjustment to promote overall safety
and develop appropriate cosmeceutical/pharmaceutical
preparations. Majority of possible side effects of TTO can be
reduced by appropriate formulations.
Beside acute reactions, theoretically, chronic subtle
cutaneous irritation can also lead to transient or permanent
cutaneous changes such as hyperpigmentation. However,
there is no data about the chronic (>12 months) dermatologic
side effects of TTO in the literature.[10] Similarly, no study
assessed the adverse events of chronic TTO use in subjects with
blepharitis, and all studies applied the treatment for 1–8 weeks.
Therefore, the absence of long‑term follow‑up also prevents us
to generalize our finding for long‑term users although we did
not detect any adverse effect of TTO in short‑term.
Some agents such as hyaluronic acid, vitamin B5, and aloe
might synergistically interact with TTO in the eyelid cleansing
products. These agents are used in Blephamed eye gel, as well.
Hyaluronic acid is a well‑known natural polysaccharide with
unique viscoelastic, moisturizing, soothing, regenerative, and
antibacterial properties that, in combination with TTO, could
help alleviate ocular discomfort in patients with anterior
blepharitis.[30,31] In addition, hyaluronic acid has potential
anti‑inflammatory properties in various inflammatory
conditions.[30] Vitamin E and B5 have moisturizing properties.
Aloe has antibacterial and anti‑inflammatory activities and have
been shown to reduce the presence of Demodex mites in the
eyelid margin and improve the signs and symptoms of chronic
blepharitis.[32] Patients who used a phospholipid–liposome
solution specially designed for lid scrub demonstrated a
significantly greater clinical improvement than those who used
a mild baby shampoo.[20] The ORONAL LCG is another main
component of Blephamed eye gel. It is a mild anionic surfactant
with its exceptional skin and ocular tolerance. This material is
specially adapted for fragile skin and mucous membranes. It’s
excellent for lifting and suspending particulate soils, crusts, and
oil. At the concentrations used, ORONAL LCG was completely
non‑irritant.
Encouraging long‑term use of eyelid hygiene presents a
challenge for the ophthalmologist.[33] Similar to long‑term
treatment adherence for other chronic asymptomatic
conditions, the compliance with everyday lid hygiene could
be a demanding task.[34] Approximately half of the patients
had good compliance with lid hygiene.[35] The reasons for
incompliance for lid hygiene are divided into patient‑centered
and procedure‑related factors.[35] Regarding patient centered
factors, a lack of time, uncomprehending the disease, concerns
about other systemic conditions, and forgetting are the
most common reasons.[35] As for procedure‑related factors,
complexity of the regimen and difficulty in remembering the
steps of the regimen were the primary reasons.[35] Theoretically,
a straightforward technique should provide better lid hygiene
compliance.[33] Therefore, the compliance rate would be
improved if the lid hygiene protocol is modified to obtain the
simplest effective regimen. Blephamed seems to be simpler and
easier technique comparing to standard treatment.
Current study has some limitations. First, it was not
known if patients were positive for Demodex mites. Second,
compliance of the patients was not evaluated by a valid tool.
Conclusion
In conclusion, current study has shown that the combination
of 2% TTO with vitamins and essential plant oils effectively
reduced anterior blepharitis severity. In addition, none of
the adverse effects reported for the existing cosmeceutical/
pharmaceutical formulations containing higher concentration
of TTO were observed in this study.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Putnam CM. Diagnosis and management of blepharitis: An
optometrist’s perspective. Clin Optom (Auckl) 2016;8:71‑8. - Pflugfelder SC, Karpecki PM, Perez VL. Treatment of blepharitis:
Recent clinical trials. Ocul Surf 2014;12:273‑84. - Duncan K, Jeng BH. Medical management of blepharitis. Curr
Opin Ophthalmol 2015;26:289‑94. - Carson CF, Hammer KA, Riley TV. Melaleuca alternifolia (Tea tree)
oil: A review of antimicrobial and other medicinal properties. Clin
Microbiol Rev 2006;19:50‑62. - Tighe S, Gao YY, Tseng SC. Terpinen‑4‑ol is the most active
ingredient of tea tree oil to kill demodex mites. Transl Vis Sci
Technol 2013;2:2. - MessaoudR, Fekih LE, MahmoudA, Amor HB, BannourR, Doan S,
et al. Improvement in ocular symptoms and signs in patients with
Demodex anterior blepharitis using a novel terpinen‑4‑ol (2.5%)
and hyaluronic acid (0.2%) cleansing wipe. Clin Ophthalmol
2019;13:1043‑54. - Cheung IMY, Xue AL, Kim A, Ammundsen K, Wang MTM,
Craig JP. In vitro anti‑demodectic effects and terpinen‑4‑ol
content of commercial eyelid cleansers. Cont Lens Anterior Eye
2018;41:513‑7. - Su CW, Tighe S, Sheha H, Cheng AMS, Tseng SCG. Safety and
efficacy of 4‑terpineol against microorganisms associated with
blepharitis and common ocular diseases. BMJ Open Ophthalmol
2018;3:e000094. - Alver O, Kıvanç SA, Akova Budak B, Tüzemen NÜ, Ener B,
Özmen AT. A clinical scoring system for diagnosis of ocular
demodicosis. Med Sci Monit 2017;23:5862‑9. - Scientific Committee on Consumer Products (SCCP). Opinion
on tea tree oil. 2008. Available from: https://www.google.
com/url?sa=t&source=web&rct=j&url=https://ec.europa.eu/
health/ph_risk/committees/04_sccp/docs/sccp_o_160.
pdf&ved=2ahUKEwiouZrRj7_9AhXGjqQKHXDjA7AQ
FnoECBQQAQ&usg=AOvVaw2JdyXfsblE4fS0CXjj
Fwqq. [Last accessed on 03 March 2023]. - Holland EJ, Mannis MJ, Lee WB. Ocular Surface Disease: Cornea,
Conjunctiva and Tear Film. London: W.B. Saunders; 2013. - Ficker L, Ramakrishnan M, Seal D, Wright P. Role of cell‑mediated
immunity to staphylococci in blepharitis. Am J Ophthalmol
1991;111:473‑9. - Kabatas N, Dogan AS, Kabatas EU, Acar M, Bicer T, Gurdal C.
The effect of demodex infestation on blepharitis and the ocular
symptoms. Eye Contact Lens 2017;43:64‑7. - Gao YY, Di Pascuale MA, Li W, Liu DTS, Baradaran‑Rafii A,
Elizondo A, et al. High prevalence of Demodex in eyelashes with
cylindrical dandruff. Invest Ophthalmol Vis Sci 2005;46:3089‑94. - Amescua G, Akpek EK, Farid M, GarciaFerrer FJ, Lin A, Rhee MK,
et al. American Academy of Ophthalmology Preferred Practice
Pattern Cornea and External Disease Panel. Blepharitis Preferred
Practice Pattern®. Ophthalmology 2019;125:5693.
- Lindsley K, Matsumura S, Hatef E, Akpek EK. Interventions for
chronic blepharitis. Cochrane Database Syst Rev 2012;16:CD005556. - Key JE. A comparative study of eyelid cleaning regimens in chronic
blepharitis. CLAO J 1996;22:209‑12. - Jackson WB. Blepharitis: Current strategies for diagnosis and
management. Can J Ophthalmol 2008;43:170‑9. - Sung J, Wang MTM, Lee SH, Cheung IMY, Ismail S, Sherwin T, et al.
Randomized double‑masked trial of eyelid cleansing treatments
for blepharitis. Ocul Surf 2018;16:77‑83. - Khaireddin R, Hueber A. Eyelid hygiene for contact lens wearers
with blepharitis. Comparative investigation of treatment with
baby shampoo versus phospholipid solution. Ophthalmologe
2013;110:146‑53. - Polack FM, Goodman DF. Experience with a new detergent lid
scrub in the management of chronic blepharitis. Arch Ophthalmol
1988;106:719‑20. - Gao YY, Xu DL, Huang J, Wang R, Tseng SC. Treatment of ocular
itching associated with ocular demodicosis by 5% tea tree oil
ointment. Cornea 2012;31:14‑7. - Maher TN. The use of tea tree oil in treating blepharitis and
meibomian gland dysfunction. Oman J Ophthalmol 2018;11:11‑5. - Lee SY, Chen PY, Lin JC, Kirkby NS, Ou CH, Chang TC. Melaleuca
alternifolia Induces Heme Oxygenase‑1 expression in Murine
RAW264.7 Cells through activation of the Nrf2‑ARE pathway. Am
J Chin Med 2017;45:1631‑48. - Kim JT, Lee SH, Chun YS, Kim JC. Tear cytokines and chemokines
in patients with Demodex blepharitis. Cytokine 2011;53:94‑9. - Hart PH, Brand C, Carson CF, Riley TV, Prager RH, Finlay‑Jones JJ.
Terpinen‑4‑ol, the main component of the essential oil of
melaleuca alternifolia (tea tree oil), suppresses inflammatory
mediator production by activated human monocytes. Inflamm
Res 2000;49:619‑26. - Qiu TY, Yeo S, Tong L. Satisfaction and convenience of using
terpenoid‑impregnated eyelid wipes and teaching method in
people without blepharitis. Clin Ophthalmol 2018;12:91‑8. - De Luca A, Carnevali A, Scalzo GC, Piccoli G, Bruzzichessi D,
Scorcia V. Efficacy and safety of wet wipes containing Hy‑Ter®
solution compared with standard care for bilateral posterior
blepharitis: A preliminary randomized controlled study.
Ophthalmol Ther 2019;8:313‑21. - Koo H, Kim TH, Kim KW, Wee SW, Chun YS, Kim JC. Ocular
surface discomfort and Demodex: Effect of tea tree oil eyelid scrub
in Demodex blepharitis. J Korean Med Sci 2012;27:1574‑9. - Brjesky VV, Maychuk YF, Petrayevsky AV, Nagorsky PG. Use of
preservative‑free hyaluronic acid (Hylabak) for a range of patients
with dry eye syndrome: Experience in Russia. Clin Ophthalmol
2014;8:1169‑77. - Rah MJ. A review of hyaluronan and its ophthalmic applications.
Optometry 2011;82:38‑43. - Vecchione A, Celandroni F, Lupetti A, Favuzza E, Mencucci R,
GhelardiE. Antimicrobial activity of a new aloevera formulation for the
hygiene of the periocular area. J Ocul Pharmacol Ther 2018;34:579‑83. - Benitez‑Del‑Castillo JM. How to promote and preserve eyelid
health. Clin Ophthalmol 2012;6:1689‑98. - Geerling G, TauberJ, Baudouin C, Goto E, Matsumoto Y, O’Brien T,
et al. The international workshop on meibomian gland dysfunction:
Report of the subcommittee on management and treatment
of meibomian gland dysfunction. Invest. Ophthalmol Vis Sci
2011;52:2050‑64. - Chuckpaiwong V, Nonpassopon M, Lekhanont K, Udomwong W,
Phimpho P, Cheewaruangroj N. Compliance with lid hygiene in
patients with meibomian gland dysfunction. Clin Ophthalmol
2022;16:1173‑82.